Core Stabilization Exercises+Voice, VOXFIT® Feature in Voyager PHX Magazine, What is Laryngeal MMP?, Abs or Lungs?, SLPs+Vocal Fatigue, and PYV!
Enjoy some educational & inspiring blog reading & be sure to roll your shoulders & focus on allowing full-body breathing as you do! Make it a GREAT day. YOU are worthy and YOU (and YOUR VOICE) are BEAUTIFUL. #DONTFORGETIT 
Core Stabilization and Vocal Performance...
VOICE production requires coordination of multiple bodily systems, including the incorporation of CORE muscles, which play a crucial role in BREATH CONTROL and VOCAL STABILITY. ![]()
![]()
New research on the CORE’s effect on VOICE? YES PLEASE! Yildiz et al. (2025) did a study with music students (divided into two groups—an experimental group (17) and a control group (10). The experimental group participated in a 10 week long core stabilization program (with PT supervision) while the control group did not receive any intervention.
Assessments (before and after the program) included acoustic voice analysis, vocal performance evaluation, and muscle strength tests.
Results showed SIGNIFICANT improvements in the experimental group compared to the control group in key ACOUSTIC parameters, VOCAL PERFORMANCE, (including musicality, technique, and breath control), and CORE MUSCLE STRENGTH. Participants reported better VOCAL CONTROL, IMPROVED BREATHING, and greater singing COMFORT.![]()
The findings suggest that CORE STABILIZATION EXERCISES CAN ENHANCE VOCAL PERFORMANCE by improving RESPIRATORY CONTROL and CORE MUSCLE STRENGTH. Like I always say, the CORE is your HOUSE (front/back, side/side, top/bottom).. it’s not just the front (rectus abdominis). Integrating such exercises into vocal training programs may benefit singers and voice professionals (and in my opinion, ALL OCCUPATIONAL VOICE USERS!!!). ![]()
![]()
![]()
![]()
.
.
#voxfit #voice #occupationalvoiceuser #core #corestrength #corestabilization #research #speechpathologist #speechpathology #voicesfittoinspire #bevocallyfit #vocalfitness #bodyandvoiceconnection #chooseyourbestvoice
VOXFIT® Feature in Voyager Phoenix Magazine!...
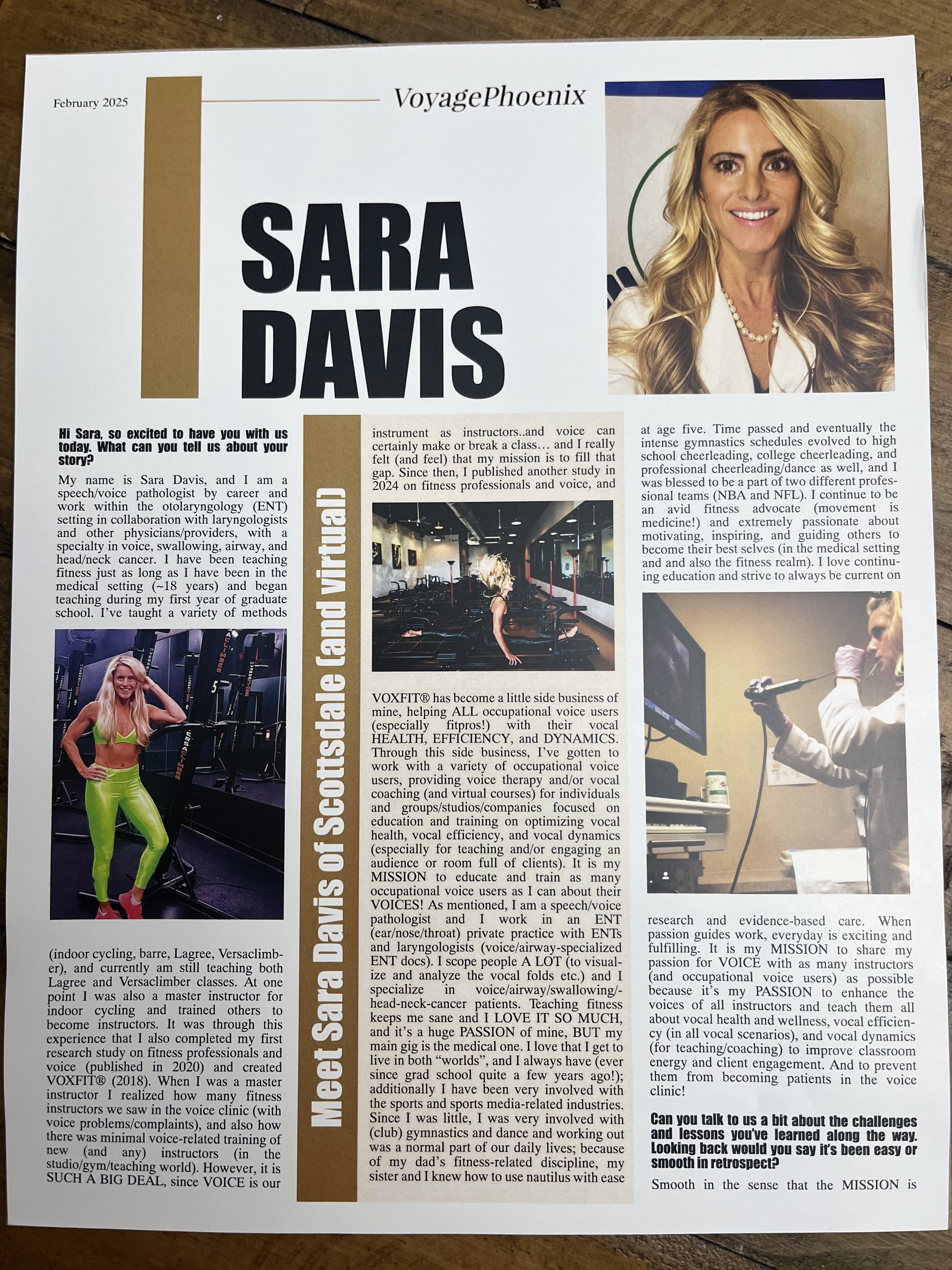
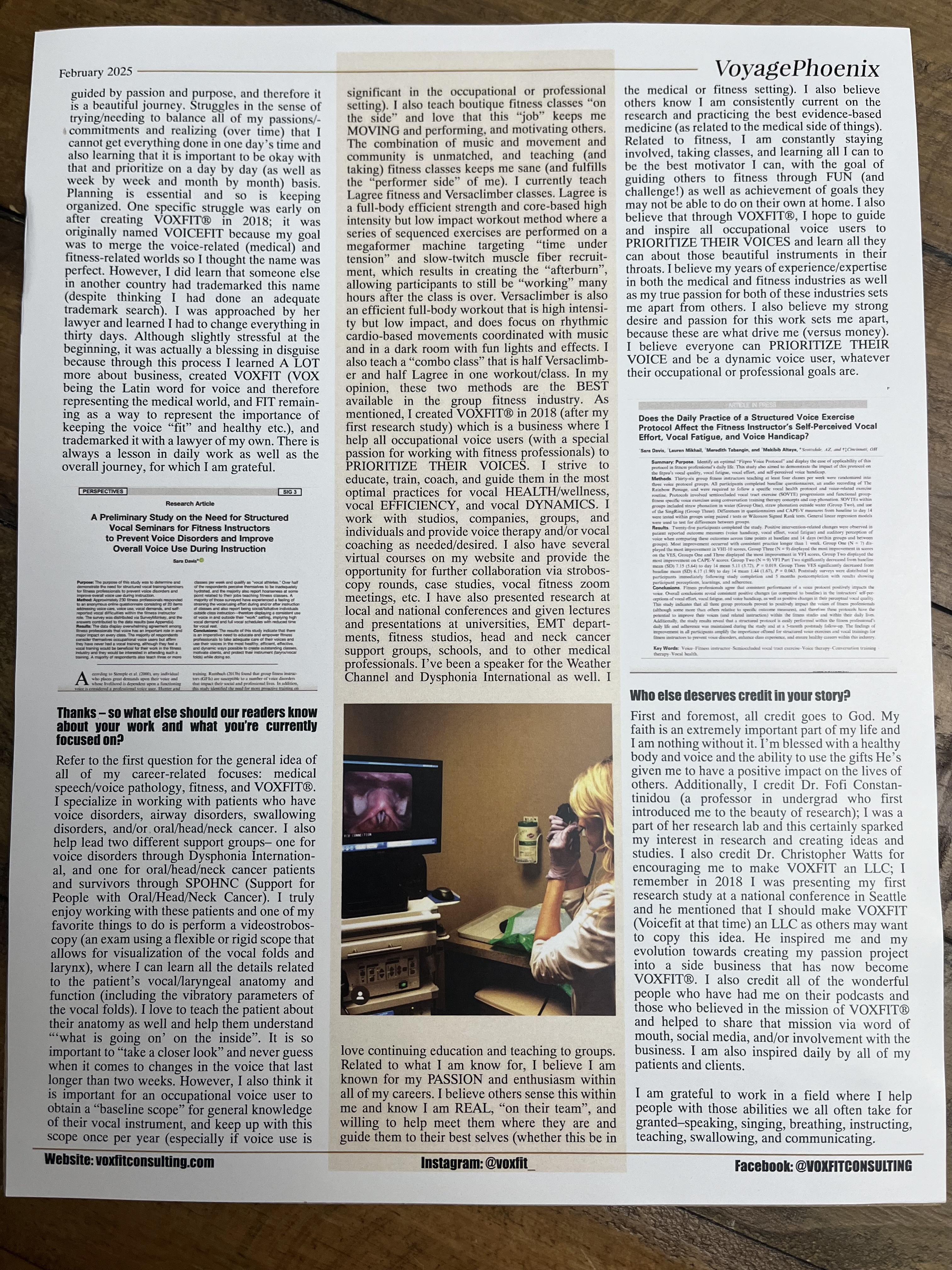
If you’ve ever wondered about me, @voxfit_ , or my journey to how I got “here”, CHECK IT OUT!! Link in bio!![]()
![]()
![]()
And as the article says, when PASSION guides WORK, every day is exciting and fulfilling! And I am SO grateful for that! I am truly grateful to work in a field where I help people with those abilities we all often take for granted—speaking, singing, breathing, instructing, teaching, swallowing, and communicating. ![]()
![]() I’m also thankful that (in more ways than one), movement IS medicine and I practice what I preach.
I’m also thankful that (in more ways than one), movement IS medicine and I practice what I preach. ![]()
![]()
![]() Oh, and I’m grateful to have learned that the purpose in life is not the final destination, but our purpose (and all the fun!) is found in the JOURNEY. It’s where the struggle is, it’s where growth begins, it’s where the magic happens
Oh, and I’m grateful to have learned that the purpose in life is not the final destination, but our purpose (and all the fun!) is found in the JOURNEY. It’s where the struggle is, it’s where growth begins, it’s where the magic happens ![]()
PRIORITIZE YOUR VOICE always. PRIORITIZE MOVEMENT always. And find JOY in the JOURNEY!![]()
![]()
.
.
.
#voxfit #voice #occupationalvoiceuser #fitness #voyagephoenixmagazine #passion #purpose #poweredbypassionandpurpose #helpothers #inspireothers #inspire #motivate #research #speechpathologist #speechpathology #voicesfittoinspire #bevocallyfit #vocalfitness #bodyandvoiceconnection #chooseyourbestvoice #gratefulheart #gratefulforthejourney
WHAT is Laryngeal MMP?!
SEE VIDEO ABOVE!!!
Ever heard of laryngeal mucous membrane pemphigoid?!!
Wanted to share a REALLY interesting case with everyone!!
The details are in the video, but overall this is about a patient who was originally scheduled with me (for a videostroboscopy—airway focused) from an outside referral… She exhibited audible stridor from the moment she walked in & had to intermittently stop to gasp for air. She was in her 80s & had never been scoped before & reportedly was told for 10 yrs that her issues were related to asthma… She verbalized to me she always said she felt it in her throat, not her chest. Long story short, she had significant supraglottic stenosis, which did turn out to be related to a confirmed diagnosis of laryngeal MMP.
MMP is a rare autoimmune disease, causing blistering & ulcerative lesions of mucous membranes. Laryngeal manifestations of MMP occur in only 5-15% of cases & are extremely rare with a prevalence of 1 in 10 million people. Untreated MMP can result in airway stenosis & obstruction. (Watters et al., 2020)
MMP is most common in the elderly with most cases in the 60-80 yrs age range. It primarily affects the oral & conjunctival mucosa, but may involve the skin, nasal mucosa, pharynx, esophagus, anogenital mucosa, & most rarely the larynx. Laryngeal involvement can lead to scarring, edema, webbing, stenosis, & airway obstruction, often leading to tracheotomy. MMP can be complicated by dysphonia &/or dysphagia & greatly impact quality of life. Studies have shown that laryngeal MMP has been successfully treated with Rituximab, allowing the patient to avoid tracheotomy. (Brake & Anthony, 2020).
YET ANOTHER case for the chronicles on the importance of TAKING A LOOK!!![]()
![]()
![]()
.
.
#voxfit, #voice, #MMP, #mucousmembrancepemphigoid #research #casestudy #speechpathologist #speechpathology #voicespecialist #airway #airwaychronicles #breathe #upperairway #takeacloserlook
ABS or LUNGS?!
Who wins? ABS or LUNGS?!
There’s not really a battle going on but an interesting new study (Baker et al., 2025) did find some evidence (as expected) that the relationships between respiratory & phonatory parameters certainly contribute to important insights for voice pedagogy, voice therapy, & vocal coaching.
Breath management techniques are key for speaking AND singing, especially in the context of performing/coaching/teaching/
Many believe there is a linear relationship where increased anterior abdominal musculature (AAM) activation will result in greater subglottic pressure (Psub) causing a rise in sound pressure level/loudness(SPL). However, the current study used surface EMG, aerodynamic, & acoustic measures to provide insights into this assumption.
3 key findings from the study include :
- In habitual behaviors of healthy singers, AAM activates
 predominantly in association with decreasing % of vital capacity
predominantly in association with decreasing % of vital capacity
- AAM activity is not strongly correlated with subglottic pressure or SPL/loudness

- Immediate contraction of AAM within the inspiratory reserve appears unnecessary for phonation

Per the study AAM contraction plays a less important role in pressure generating forces than previously thought, & their activation is primarily related to % of vital capacity/lung volume rather than regulating vocal intensity.
![]() The study also encourages voice professionals to consider principles of vocal ECONOMY
The study also encourages voice professionals to consider principles of vocal ECONOMY![]() , mechanical EFFICIENCY
, mechanical EFFICIENCY![]() , & INDIVIDUALITY when teaching breath management strategies to their students/clients & ensure the approach prioritizes incorporation of understanding of basic respiratory physiology.
, & INDIVIDUALITY when teaching breath management strategies to their students/clients & ensure the approach prioritizes incorporation of understanding of basic respiratory physiology.![]()
Soooo YES the abs![]() matter & YES the lungs
matter & YES the lungs![]() REALLY matter, & the prioritization of a focus on both will likely produce the best vocal outcomes for performing & more exuberant tasks. However, based on this study & other literature, if I had to prioritize one, it would certainly be focusing on expanding lung capacity/lung volume because the the abdominals are only activated once vital capacity gets to 40% or less. Why not extend the time it takes to get to that 40%? Also, as beautifully described in the BREATH book (by James Nestor), length of life in years is correlated to our lung capacity/lung expansion abilities… So if we want to live longer & speak/sing better it’s important to target this aspect of training & possibly prioritize it above a muscular-based focus. However, as mentioned, I strongly believe BOTH the lungs and the abdominals (& other body muscles!…& the skeleton! Helloooo ESTILL voice method/ANCHORING!) are incredibly important in supporting the voice… so YES, here is another beautiful reason to prioritize your voice via EXERCISE (respiratory muscle, strength training, respiratory muscle, pattern training, cardio, working out, breathing exercises, etc etc)!
REALLY matter, & the prioritization of a focus on both will likely produce the best vocal outcomes for performing & more exuberant tasks. However, based on this study & other literature, if I had to prioritize one, it would certainly be focusing on expanding lung capacity/lung volume because the the abdominals are only activated once vital capacity gets to 40% or less. Why not extend the time it takes to get to that 40%? Also, as beautifully described in the BREATH book (by James Nestor), length of life in years is correlated to our lung capacity/lung expansion abilities… So if we want to live longer & speak/sing better it’s important to target this aspect of training & possibly prioritize it above a muscular-based focus. However, as mentioned, I strongly believe BOTH the lungs and the abdominals (& other body muscles!…& the skeleton! Helloooo ESTILL voice method/ANCHORING!) are incredibly important in supporting the voice… so YES, here is another beautiful reason to prioritize your voice via EXERCISE (respiratory muscle, strength training, respiratory muscle, pattern training, cardio, working out, breathing exercises, etc etc)!![]()
![]()
![]()
.
.
#voxfit #voice #voicesfittoinspire #abs #lungs #research #bevocallyfit #chooseyourbestvoice #occupationalvoiceuser #speechpathologist #singer #speaker #vitalcapacity #lungvolume #rectusabdominis #workout #bodyvoiceconnection #vocalhealth #vocalefficiency #vocaldynamics #breathmanagement #poweredbypassionandpurpose
SLPs and Vocal Fatigue...

It’s a known fact that occupational and professional voice users are more susceptible to vocal injury, vocal fatigue, and vocal challenges in general… because of higher vocal demands and consistent need for dynamic voice use. It’s also known that vocal education and training positively impacts vocal health and longevity. It is expected that (vocal) professionals with this training will likely have less risk than others… However, a 2025 study looked into what extent SLPs adhere to vocal hygiene and healthy vocal behaviors, and how this affects vocal fatigue.
With a full schedule of back-to-back patients and constant talking all day, SLPs are certainly at higher risk for vocal fatigue, and should most definitely prioritize their voices by prioritizing several vocal hygiene-related concepts including hydration (all four ways!), vocal budget, vocal load, vocal demands, vocal schedule, optimal vocal use patterns, optimal voice placement, and use of vocal exercises. This study revealed data that the SLP community (of which I am a part) finds it quite challenging to fully practice what they preach (regarding voice-related care/hygiene and behaviors), which leads to concerning vocal fatigue levels.
Just your DAILY REMINDER that ALL occupational and professional voice users NEED to PRIORITIZE their VOICES consistently. Even the most vocally “knowledgeable” can succumb to the day to day craziness and end up in a wave of vocal exhaustion. Don’t let it be you! #prioritizeyourvoice![]()
![]()
![]()
![]()
![]()
![]()
.
.
.
#voxfit #voice #voicesfittoinspire #research #bevocallyfit #chooseyourbestvoice #occupationalvoiceuser #speechpathologist #singer #speaker #fitpro #slp #voicespecialist #vocalhealth #vocalefficiency #vocaldynamics #poweredbypassionandpurpose
PYV: Anddd of course, always REMEMBER to PRIORITIZE YOUR VOICE! ...
How are YOU prioritizing your voice today? And everyday? As an OCCUPATIONAL VOICE USER, it SHOULD be one of your top priorities!
.
What do you need to know to keep your voice healthy? You should understand how the voice works, how to protect and care for your voice, and how to use your voice and entire vocal mechanism in the most efficient, effective, and dynamic ways possible.
.
.
I’m super PASSIONATE about this population of voice users (I’m one and most of you are too!), and am HERE TO HELP! Reach out with any questions, concerns, or if you’d like to work together. Email me at [email protected] or DM me on @voxfit_ ...


